Uganda commended for malaria fight
The assembly saw Uganda join hands with fellow African nations to rally global support in the fight against malaria drug resistance—an escalating threat that risks undermining two decades of progress in malaria control at the 78th World Health Assembly (WHA) in Geneva.
The gathering marked a significant moment for Africa’s response to emerging drug resistance, particularly partial resistance to artemisinin—the core component of the first-line malaria treatment, artemisinin-based combination therapies (ACTs). (Courtesy Photo)
Uganda has been commended for its efforts in fighting malaria.
During the 78th World Health Assembly (WHA) in Geneva, Switzerland, on Tuesday, May 20, 2025, Uganda's primary healthcare state minister, Margaret Muhanga, who led the Ugandan delegation, received a badge of recognition on behalf of the Government.
The assembly saw Uganda join hands with fellow African nations to rally global support in the fight against malaria drug resistance—an escalating threat that risks undermining two decades of progress in malaria control at the 78th World Health Assembly (WHA) in Geneva.
With malaria still claiming more than 4,817 lives in Uganda annually, the country's leadership emphasised the urgent need to protect the effectiveness of existing treatments and to invest in the development of new ones.
Muhanga said, “drug resistance is not a problem we can afford to ignore. For Uganda, where malaria is still the leading cause of illness and death, we must protect the medicines that have saved millions and push for innovation that will secure future generations”.
The high-level side event, led by Rwanda and co-hosted by countries, including Uganda, South Sudan, Namibia, Eritrea and Tanzania, was supported by the World Health Organisation (WHO), the Africa Centres for Disease Control and Prevention, Medicines for Malaria Venture (MMV), and the RBM Partnership to End Malaria.
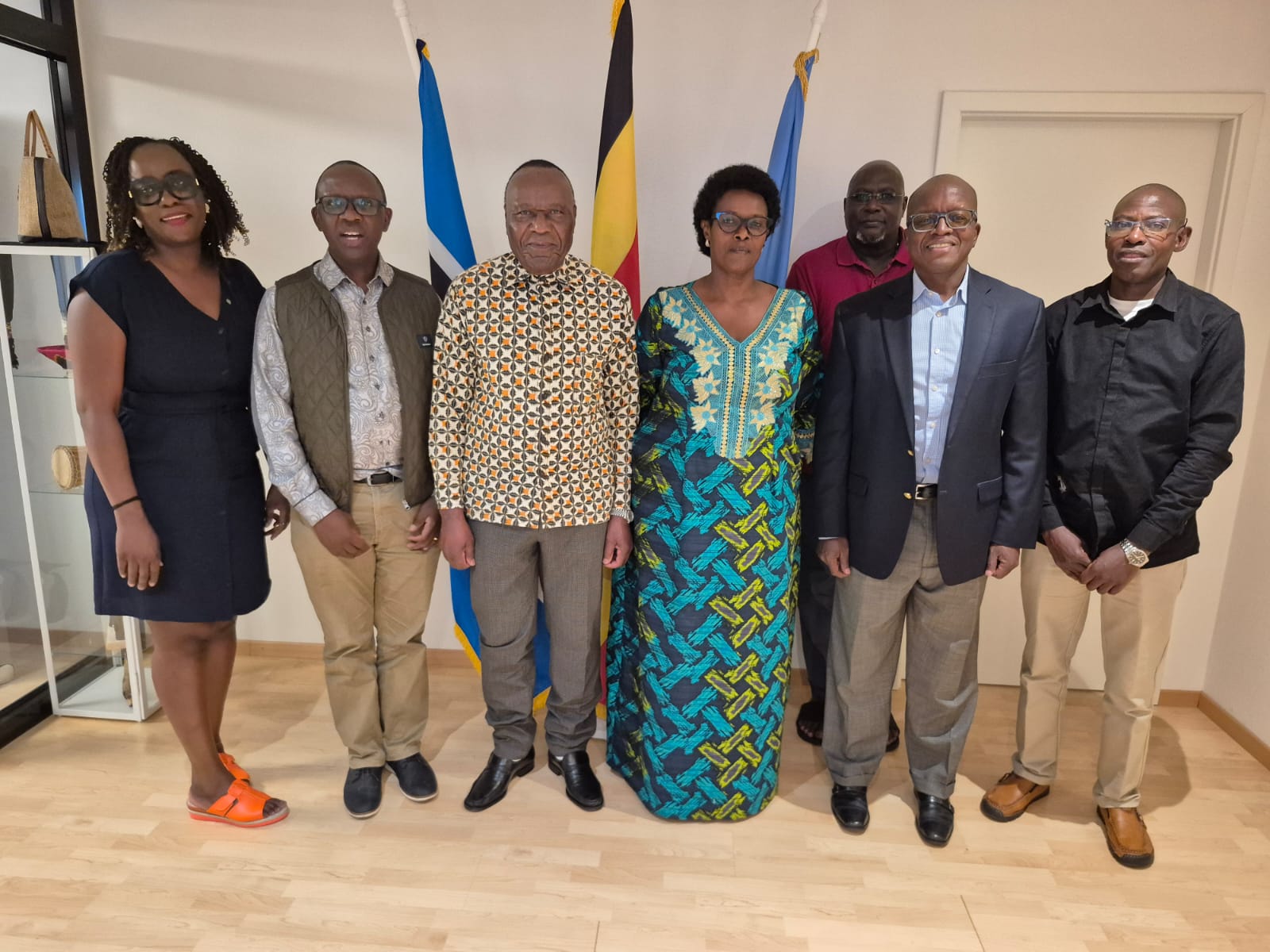
Ugandan delegation at the World Health Assembly in Geneva, led by the Minister of State for Health in charge of Primary Health Care, Margaret Muhanga. (Courtesy Photo)
The gathering marked a significant moment for Africa’s response to emerging drug resistance, particularly partial resistance to artemisinin—the core component of the first-line malaria treatment, artemisinin-based combination therapies (ACTs).
Experts warn that if drug resistance becomes widespread, Africa could see an additional 16 million malaria cases and up to 80,000 more deaths each year.
MMV’s CEO Dr Martin Fitchet described the continent's united response as a “co-ordinated, committed and united call” from African leadership, adding that the organisation is fully committed to supporting African-led strategies with scientific and operational expertise.
“Innovation is critical in the fight against drug resistance,” Dr Fitchet said. “With our partners, we’re developing next-generation antimalarials that could reach patients by 2027—while acting now to preserve the power of today’s treatments. Both are vital to outpace resistance and keep saving lives.”
The WHA also saw the launch of the Ministerial Malaria Champions initiative by the African Leaders Malaria Alliance (ALMA) and the RBM Partnership to End Malaria.
Uganda was also recognised among the inaugural cohort of countries whose health ministers will spearhead intensified efforts to eliminate malaria across the continent.
These champions are expected to secure essential resources, implement strategic plans, and promote regional collaboration to accelerate progress.
“Our inclusion in the Ministerial Malaria Champions initiative is a testament to Uganda’s commitment to fighting malaria,” Muhanga said.
Big push against malaria
Another key moment came with the launch of the next chapter of the Change the Story campaign—a collaborative effort between Malaria No More UK and Speak Up Africa.
The campaign includes a compelling short film featuring girls from Uganda, Côte d’Ivoire and Burkina Faso, showcasing the real-life impact of malaria on young people and calling for full replenishment of the Global Fund to Fight AIDS, Tuberculosis and Malaria.
Dr Astrid Bonfield, CEO of Malaria No More UK, said, “This campaign places children at the heart of the malaria response. Their voices remind us what is working, what is at risk, and why our action is urgently needed.”
Speakers throughout the event underscored the need for increased investment. The continent faces an annual malaria funding gap of $5.2 billion, and an additional $11 billion is needed to build climate-resilient health systems.
“We are encouraging these champions to come together in solidarity and help hold one another and all ministers across the continent accountable for delivering results, playing their part in changing the story and driving Africa toward zero malaria.” Said Joy Phumaphi, African Leaders Malaria Alliance (ALMA).
Uganda, like many African countries, continues to rely on donor support from institutions such as the Global Fund. Leaders warned that any reduction in funding could reverse the hard-won gains of recent years.
Dr Daniel Ngamije, Director of the Global Malaria Programme at WHO, reiterated that collective action is the only way forward.
“Drug resistance is a growing threat that demands urgent, collective action. We must act decisively and in solidarity to preserve the tools we have—and ensure access to effective malaria treatments for all in need.”
In addition to surveillance and research, Uganda is also exploring the deployment of advanced treatment strategies such as multiple first-line therapies (MFT) and triple ACT combinations (TACTs), both supported by MMV. These approaches aim to diversify and strengthen treatment regimens to make it harder for malaria parasites to develop resistance.
Uganda also launched the malaria vaccination across all highly burdened districts to all children below two years but faces a high-burden malaria country, with its entire population of 45.5 million at risk of being infected with malaria.
Vulnerable groups include pregnant women and children under five, with the highest transmission areas being northern Uganda (Acholi, Karamoja, Lango, and West Nile regions) and eastern Uganda (Busoga region). [1] As of 2022, Uganda had the 3rd highest global burden of malaria cases (5.1%) and the 8th highest level of deaths (2.9%).