Ugandan scientist honored for Bilharzia research
School children are the most affected because of their increased water contact through playing, bathing, swimming and fishing.
PIC: Prof. Virginio Ongom (right) with collegues. (File photo)
AWARDS
KAMPALA - A Ugandan scientist who made pioneering discoveries about Bilharzia (schistomiasis) got posthumous honours for his work on Thursday, June 28, 2018.
Prof. Virginio Lachara Ongom, who was the first African director of the Institute of Public Health at Makerere University between 1975 and 1980, was honoured for his extensive research into the disease.
Bilharzia, a disease caused by parasitic flatworms called schistosomes.
Transmission occurs when people suffering from Bilharzia contaminate freshwater sources with their excreta containing parasite eggs.
More than one in three Ugandans suffer from Bilharzia, according to a survey conducted by Makerere University School of Public Health in 2017.
The survey, whose findings were released early this month shows that about 11 million people in Uganda are living with the disease.
Prof Ongom, who passed away 38 years ago, left a large profile of works about the disease that was later published in several globally respected medical journals.
The School of Public Health, where most of the research was carried out, has organised a Memorial Lecture in his honour on Thursday.
The public lecture will examine efforts to tame the disease along with other neglected tropical diseases since 1980, as well as steps to eliminate them to achieve health goals under Vision 2040.
This will be under the theme "Bilharzia (schistosomiasis) and other Neglected Tropical Diseases in Uganda since 1980: Towards elimination in realisation of Uganda Vision 2040, what is the way forward.
Prof. Ongom's research was pioneer work on Bihharzia in Uganda, which informed policy formulation and initial response to Bilharzia for this country.
According to the Dean School of Public Health Makerere University School Professor Rhoda Wanyenze, Ongom's research generated much interest in Bilhazia in Uganda and interest in having it eliminated.

Prof. Ongom with other UCB board members. (File photo)
In 2003 Uganda become the first African countries to launch a national-scale bilharzia and intestinal worm control programme.
"We are going to use the memorial lecture not only to recognise his work in the field of bilharzia but, use the occasion to raise attention the disease which is still a problem," Professor Wanyenze said.
Prof Birgitte Vennervald, from the University of Copenhagen will be the Guest Speaker at the event which will take place at Makerere University main hall.
While in his home district of Pakwach, the health centre IV is also to be renamed after him on June 30, 2018 in honour of his dedication to combating bilharzia in the area.
Discovering Bilharzia in Uganda
In 1902, the first case of bilharzia was first observed and reported in Kuluva hospital Arua District north of Uganda.
It was discovered in a hospitalized patient with sleeping sickness.
Despite this discovery, it was not until 1923 and 1924 respectively that a high incidence of Bilharzia was noted in the West Nile region, north of Uganda.
It was found that the prevalence and intensity of infection was highest immediately along the banks of the River Nile and decreased with altitude and distance from the Nile.
A similar observation was reached indicating that altitude and distance influence the distribution of Bilharzia in Lake Bunyonyi in Kabale in Western Uganda.
Also observed was that enlarged spleens and anaemia were a common clinical feature among children around ten years old with high intensity of bilharzia infection.
In the 1970s Professor Virginio Lachara Ongom (RIP) dedicated his medical expertise and studied and documented the epidemiology and consequence of bilharzias (schistosomiasis) infection among Jonam.
The Jonam are of the Alur tribe, (a Luo ethnic group), living in fishing villages of Panyagoro and Panyimur, in Nebbi District, in West Nile, North of Uganda.
Ongom carried out a survey to determine the incidence, distribution and clinical significance of bilharzia.
A study of age and sex incidence in 1, 651 persons in the Nile valley and 3, 327 persons in the Western Uplands showed a generally higher infection rate in males.
Under the age of three years only two out of 320 children examined were found infected.
The highest incidence was in the age group 5-15 years.
Frequently on his return home to Kampala, he would return with his patients with swollen stomachs for some few days before relocating them to Mulago hospital.
"I believe the patients who were brought to Kampala were the ones whose conditions could not be handled in the village since the medical teams used to treat many at Pakwach health and various locations in Jonam particularly along the river Nile," his wife Cecilia Ongom says.
In Panyagoro village where Ongom hailed from, the treatment was being done under his neem tree that he planted having brought the tree seedling from India.
His children had to bear with his work, knowing that he was a Doctor. For Cecilia Ongom, it was always satisfying to see many of his patients brought to Kampala looking fine back in the village.
Today Eastern Uganda has the most cases of according to a new survey done by the Health Ministry and Makerere School of Public health.
It was found that four out of every 10 children and three of every adult in Uganda present with bilharzia.
Bilharzia is mainly found in 73 districts around large water bodies as Lakes Victoria, Kyoga, Albert and River Nile.
School children are the most affected because of their increased water contact through playing, bathing, swimming and fishing.
If left untreated, bilharzia can cause damage to internal body organs such as the liver, bladder and the kidneys, leading to death.
But, bilharzia is completely treatable, preventable and even curable but, it is still a major concern in most parts of Uganda.
Ongom's journey to medicine, the army and back to medicine.
Uganda's former Prime Minister Kintu Musoke was one of Ongom's closest friends when he got to medical school.
"I met him in India when we were offered the government of India scholarships after high school," Kintu Musoke reveals.
Jawaharlal Nehru who was the first Prime Minister of India and a central figure in Indian politics before and after independence had handed out these scholarships.
He was of the view that African countries needed cadres in different fields including economics and politics in preparation for independence.
Therefore every year, 10-12 people were offered scholarships to study various courses in India. "In 1959, Ongom and I were among the lucky recipients of this scholarship," Kintu Musoke discloses.
"Ongom travelled to India to study medicine and I had traveled to India to study political Science.
The two met at the Delhi College of Delhi University. Ongom did pre-med as required before joining medical college. Kintu Musoke on the other hand was doing a BA honours in Political Science.
"We were staying in the same hostel which was the Delhi College hostel that's where we struck a friendship. Ongom, on completing his pre-med in the first year was accepted to join Agra medical college," Kintu Musoke narrates.
"Ours was to support the country grow by being in the main political movement but also by infiltrating all other organs of government so that we would have our own people to represent our shared views," Kintu Musoke recounts.
He states Ongom was very intelligent, studious, hardworking, made a niche for himself in medicine and made a lot of contributions to the school of health writing so many papers on medicine.
These were people with the same ideology with the country at heart.
"We positioned ourselves to be everywhere; our intention was to take over the leadership of this country," he reveals.
"So when we came back we persuaded Ongom to join the army to represent our ideology and push our agenda. He was there with another colleague, Dr Aston Bonde.
We aspired to be in prisons, police and the civil service, so we pushed people there too," he adds.
Once in these positions in case there was an opening for an administrative position or for promotion the group fronted and put their own.
As a result whenever any change was being fronted, their own people would be there to represent them and to ensure their vision was being put across.
But, later on when Amin took power, the group realized that he did not want educated people. "We agreed with Ongom to move from the army to public health but, once he joined public health, he found a profession for himself that he pursued diligently," Kintu Musoke reveals.
But, Musoke says ongom was very political too. Before he travelled to India, as a student at the Royal Technical College/Royal College Nairobi (now University of Nairobi) he had met with Milton Obote.
So when Obote was elected as leader of Uganda's People's Congress (UPC) "he introduced his friends to him and that's how we came to support UPC," Kintu Musoke narrates.
Our common world outlook is how we joined up with Museveni in leadership and it also kept us together," Kintu Musoke explains.
In that sense, Ongom exercised his capacity for the good of his country, serving in the army and becoming the first black Dean of the school of public health at Makerere University,
"For him country came first before his interest. He was always rising and left the army as a captain a position he maintained even after joining Makerere University.
Wherever he was placed to work, he made his presence felt by serving the people and putting their interest first. We miss him," Kintu Musoke acknowledges.
Unfortunately at the time Amin was removed from power Ongom suffered a stroke. Unfortunately he died of a complication when he was being taken to the UK for treatment.
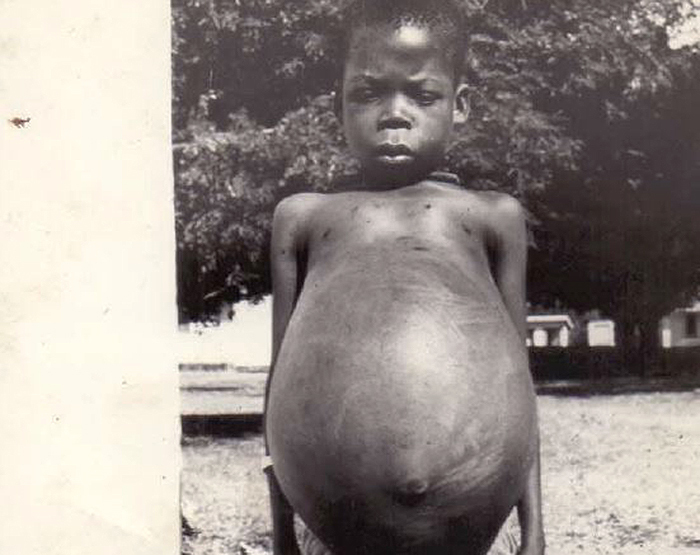
A photo of a bilharzia patient. In Panyagoro village where Ongom hailed from, the treatment was being done under his neem tree. (File photo)
Impact of Ongom's work, his legacy and future plans
Prof. Wanyenze says back then Uganda didn't have many people conduct research on Bilharzia.
"Prof. Ongom's work generated much interest in the disease in Uganda and interest in having it eliminated," she says.
In 2003 Uganda become the first African countries to launch a national-scale bilharzia and intestinal worm control programme in Pakwach in Jonam County the area where he conducted his initial research.
But bilharzia is still seen as the second most devastating parasitic disease in the world after malaria.
By the year 2000, the disease was claiming about 200,000 people annually, according to World Health Organisation.
A recent nationwide study shows 29% prevalence of bilharzia which means one person in every three has the disease.
Dr. Simon Kibira, a lecturer at the Makerere University's department of community health and behavioral sciences, says open defecation and urination are major risk factors in the spread of Bilharzia.
The latest survey indicates bilharzia is more common among children between the age of two and four years (41.9%) and pregnant women (20%).
Its prevalence is highest in eastern Uganda (34.7%), followed by Northern Uganda (30.9%), Central (29.5%) and Western Uganda (23.6%).
Prof. Wanyenze says Uganda is a country with one of the highest prevalence rates of Bilhazia in the world.
"We are doing badly especially in some districts around Lake Kyoga," she says.
The 2015 study by Makerere University School of Public Health around eight districts of Lake Kyoga put the prevalence at 48.5%.
This means one in every two people has bilhazia. "This is not acceptable. We have a very high national prevalence rate of bilharzia.
Actually people even don't know they have the disease. They have children looking different with swollen tummies but will not know it is bilharzia because they are not diagnosed," she says.
Wanyenze says government needs to act now on some of the research findings on Bilhazia so that we can eliminate bilharzia.
Bilharzia is a disease targeted by World Health Organisation for elimination in many countries including Uganda by 2020.