Screen regularly to escape cervical cancer
Mar 20, 2024
Cervix cancer is the most prevalent among women. Birungi says most women visit the facility when they are at stages three and four - quite advanced – where there are limited chances of a cure.

An Intensive care unit of Mulago Specialised Women and Neonatal Hospital (MSWNH). (Photo by Moses Nsubuga)

Jacky Achan
Journalist @New Vision
_______________
Cervical cancer has a pre-cancer lesion or abnormality, which means that it takes long to manifest as cancer.
Although preventable, it kills women. “The pre-cancer stage can be identified, treated, and the patient monitored so that the cancer does not develop,” Dr Juliet Birungi, a consultant gynaecological oncologist working with Mulago Specialised Women and Neonatal Hospital (MSWNH) says.

However, most women are not in the habit of screening for abnormalities in their genitalia that could become cancerous. Birungi says the vulva, vagina, and cervix will have some pre-cancer abnormalities.
Why the concern?
Cervix cancer is the most prevalent among women. Birungi says most women visit the facility when they are at stages three and four - quite advanced – where there are limited chances of a cure.
It is unfortunate that the pre-cancer abnormalities are there, but most women will not have them checked, allowing the cancer to develop.
According to the BMC Cancer Journal, Uganda has the seventh-highest incidence rate of cervical cancer globally and the second-highest in East Africa, with a rate of 28.8 cases per 100,000 people per year.
The annual incidence of cervical cancer is reported to be 6,959 cases, with a corresponding mortality rate of 4,607 deaths.

Simon Mukasa Senior Lab technician looking through a multi head microscope which is also used in teaching and peer view by many pathologists for examining tissues. (Photo by Moses Nsubuga)
Cervical cancer is the number one cause of cancer-related deaths in women in Uganda.
The Human papillomavirus (HPV) is responsible for over 90% of cervical cancer cases. The majority of people get HPV at the time they initiate sexual intercourse, but the majority will clear the virus, explains Birungi.
“However, there are people who do not clear the virus; and are at risk of developing those precancer abnormalities that could later progress to cervical cancer,” she says.
So, who are the people who fail to clear the virus and are at risk?
These are people who smoke, those who engage in sex early - before 21 years, people with multiple sex partners or those with a partner with multiple sex partners.
There are also those with HIV/AIDS and people who are immunosuppressed.
Screening
When tests are conducted depending on what is found, a decision is made on whether to treat or follow up, depending on the different abnormalities.
“We have a robust screening programme for HIV positives because they are at high risk of getting cervical cancer. We utilise the screen and treat protocol. This means that at the point when cervical cancer is screened for if an abnormality is found, it is treated to avoid loss of follow-up.

Senior Lab technician, Simon Mukasa showing a hormone analysis or hormone profile machine which is also used for infertility check at the Mulago Specialised Women and Neonatal Hospital. (Photo by Moses Nsubuga)
“The challenge is that when you test someone and tell them to come back after two weeks for their results, they do not. To avoid that kind of lost follow-up, we adopted the screen and treat method,” Birungi reveals.
“The MSWNH has a screening clinic where women can walk in and screen. Also, it offers opportunistic screening, which means that before a patient receives a service like family planning or any surgical operation for any condition, we offer screening for cervical cancer first,” Birungi says.
Whereas it may not require written consent, verbal consent is paramount because the procedure is intrusive.
“How do I get to your private parts without your permission?” the doctor asks.
Diagnosis and treatment for cervical cancer
“Many people come to the hospital with a discharge, which may not be cancer, but if it is too much, smelly, and persistent, a test will be done,” Birungi says.
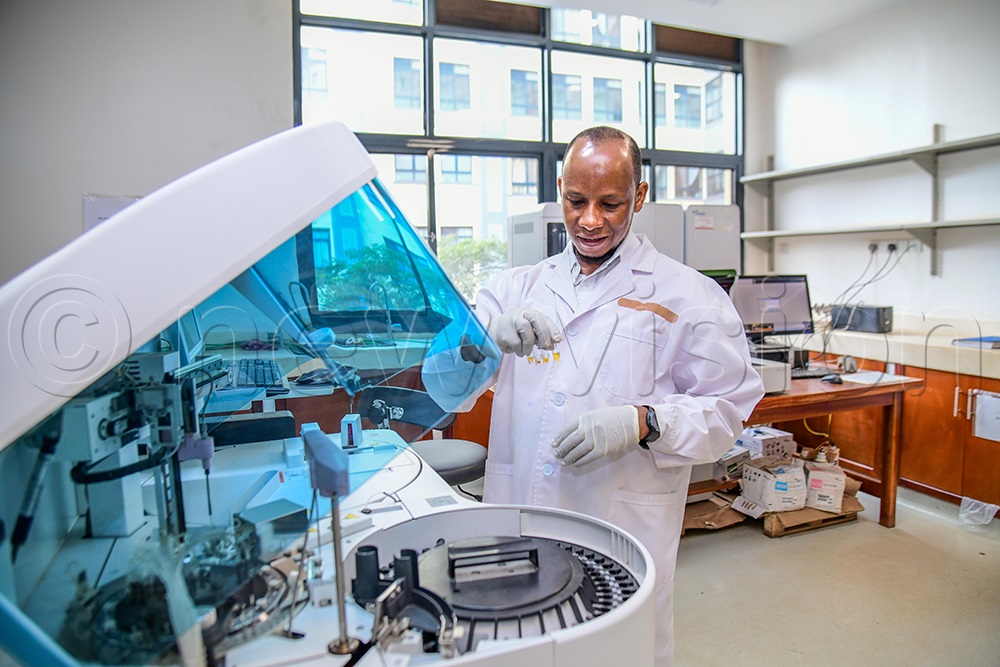
Senior Lab technician, Simon Mukasa showing a special chemistry test machine at Mulago Specialised Women and Neonatal Hospital (MSWNH). (Photo by Moses Nsubuga)
She also says people can bleed during intercourse, menopause, or between menstrual cycle periods (below 21 days). “By the time they start having pain in the lower abdomen, the cancer is quite advanced.”
She appealed to women to screen for cervical cancer and also report early in case of symptoms for early detection. “Let the cancer be detected early so we can treat it when the chances of cure are high,” Birungi says.
She adds: “The tenets of managing cancer are three: surgery, chemotherapy, and radiotherapy. We can use one or a combination of all three, depending on the stage of cancer.
Surgery is usually for cancer at an early stage. However, if the patient needs chemotherapy or radiotherapy, then we can refer them to the Uganda Cancer Institute (UCI).
The institute has a department of gynaecological oncology and radiation oncology that deals with women’s cancers. We collaborate with them to care for women with cancer.
MSWNH also works in collaboration with UCI to train super-specialist doctors in the field of women’s cancer.
Cervical cancer: primary and secondary preventive measures
The Human Papilloma Virus (HPV) vaccination for girls between the ages of nine and 14 years is the most plausible preventive method.
The Government provides it as part of the immunization schedule.
“We chose that age because we presume that they haven’t yet initiated sexual intercourse, hence have not been exposed to the HPV, and their immune response to vaccination is great. They normally get two doses. We also have a catch-up vaccination for those 15 to 26 years old.

Mammogram machine at Mulago Specialised Women and Neonatal Hospital (MSWNH). (Photo by Moses Nsubuga)
“Not that the vaccine prevents them from getting the virus, but it protects them from pre-cancer abnormalities that will progress to cancer. It is over 90% protective. It has been tested and proven as an effective way of preventing cervical cancer,” she says of primary preventive measures.
Birungi also advises women to avoid early sexual intercourse, smoking and multiple sex partners.
Secondary prevention measures
This happens when the virus has been acquired. Screening is done for the age of 25 and above. It includes:
Pap smear: This is given to women aged 25 and older.
Visual Inspection of the Cervix with Acetic Acid (VIA) is another effective, inexpensive screening test that can be combined with simple treatment procedures for early cervical lesions.
“We commonly use vinegar, applying it to the mouth of the womb (cervix), observing any changes that could signify those abnormalities. If there are changes, then the patient is treated,” states Birungi.
Visual Inspection with Lugol’s Iodine (VILI) is another preventive measure. It was the first method used for cervical cancer screening, introduced in the 1930s.
“We put iodine in the mouth of the womb (cervix); if it’s normal, there is a different way it stains. If it’s abnormal, it stains yellow (mustard yellow). It shows those abnormalities that we can treat,” Birungi says.

An Intensive care unit of Mulago Specialised Women and Neonatal Hospital (MSWNH). (Photo by Moses Nsubuga)
She adds that the visual inspections and pap smears are done every three years, if normal.
HPV DNA testing is the other alternative. An HPV DNA test is done to determine if someone has the actual HPV virus, and if normal, it is repeated after five years. If it is positive, further testing and treatment can be done.
“This test has a very high reliability. HPV tests are not done for women under 30 years because many people will have infections in their early sexual lives, which would otherwise clear,” Birungi says.

No Comment