Fasting in Ramadan: The dos and don’ts
Fasting for patients with diabetes represents an important personal decision that should be made in light of guidelines for religious exemptions and after careful consideration of the associated risks in consultation with health care providers.
Fasting in Ramadan: The dos and don’ts
____________________
OPINION
By Prof. Silver Bahendeka and Sheikh Muhammad Ali Waiswa
Ugandan Muslim Community have joining the rest of the world to observe the Holy Month of Ramadan.
During this month of Ramadan, able-bodied Muslims fast from dawn until sunset, refraining from eating, drinking and smoking. Ramadan is profoundly spiritual and of great importance in the Muslim community.
The fasting period occurs 29 - 30 days, in alignment with the lunar calendar. Ramadan is also a time of communal prayers, family gatherings, and sharing of meals, which brings spiritual and social benefits, but can also present unique health challenges.
Fasting may raise important questions for people with health conditions such as diabetes, for pregnant women, and others who may be at risk.
However, by following simple guidelines, people who may be at risk can stay healthy and keep safe while they fast (World Health Organization at: https://www.emro.who.int/media/media-events/ramadan-2026.html; & Ibrahim M, et al. Recommendations for the Management of Diabetes During Ramadan Applying the Principles of the ADA/ EASD Consensus: Update 2025. Diabetes Metab Res Rev. 2025 Jul;41(5): e70057. doi: 10.1002/dmrr.70057. PMID: 40512040).
Before these great strides were taken, especially in the management of diabetes, patients with health conditions were initially considered not able to observe this holy month, creating significant frustration and disconnect with their families and loved ones.
As patient outcomes improved through the emergence of better pharmacotherapy and increasing technology, the restrictions related to diseases have been reconsidered.
Health workers need to talk to your patients and plan. Medications need to be rescheduled to fit non-fasting hours.
- 1x Daily Meds: Typically taken at sunset or pre-dawn
- 2x Daily Meds: One dose at iftar (meal at sunset) second dose at suhoor (pre-dawn meal)
- 3x Daily Meds: These regimens may be require switching to long-acting formulations or alternatives
Conditions requiring careful adjustment in consultation with the health provider
- Diabetes:
- Risk of hypoglycaemia (low sugar) during fasting hours, and hyperglycaemia (high sugar) after evening meal
- Shift to long-acting insulin or reduce doses to prevent nocturnal (night) hypoglycaemia
- Continuous glucose monitoring is recommended
- Hypertension:
- Adjust antihypertensive medication to ensure 24-hour blood pressure control
- Diuretics should be avoided during fasting hours to prevent dehydration
- Gastrointestinal Disorders:
- Acid reduction medication (PPI’s, H2 blockers) can be taken before suhoor (pre-dawn meal) or at ifter (sunset meal) to prevent heart burn
- Acid reduction medication (PPI’s, H2 blockers) can be taken before suhoor (pre-dawn meal) or at ifter (sunset meal) to prevent heart burn
- Epilepsy:
- Switch to long-acting anti-epileptic drugs to maintain steady levels during fasting hours
- Switch to long-acting anti-epileptic drugs to maintain steady levels during fasting hours
- Other chronic illnesses:
- Asthma, Kidney disease, gastrointestinal, and anti-psychotics may require individualised plans.
Health Providers: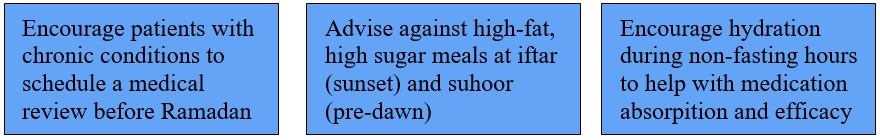
To the health worker, it is important to prioritise both safety and cultural sensitivity in treatment plans for managing type 2 diabetes during Ramadan.
There are several dimensions of quality of life to address during these conversations with patients, including the following: emotional, social and cognitive functions.
This is why the planning of fasting should be done early to give these assessments time to be done and executed and, therefore, should never present as emergencies during the fasting period.
Fasting
Fasting during Ramadan, a holy month of Islam, is a duty for all healthy adult Muslims. Ramadan is a lunar-based month, and its duration varies between 29 and 30 days.
Muslims who fast during Ramadan must abstain from eating, drinking, use of oral medications, and smoking from pre-dawn to after sunset; however, there are no restrictions on food or fluid intake between sunset and dawn.
Most people consume two meals per day during this month, one after sunset (Iftar) and the other before dawn (Suhoor or Daku named after Kigoma kya Daku in East Africa). Fasting is not meant to create excessive hardship on the Muslim individual according to religious tenets.
Nevertheless, many patients with diabetes insist on fasting during Ramadan, thereby creating a medical challenge for themselves and their health care providers.
It is for this important reason that health care professionals should be knowledgeable on the effects of fasting on diabetes.
Very comprehensive recommendations for management of diabetes in patients who elect to fast during Ramadan were proposed in 1995 at a conference in Casablanca.
However, fasting, especially among patients with type 1 diabetes (Insulin Dependent Diabetes; Juvenile Onset Diabetes) with poor diabetes control, is associated with multiple, occasionally life-threatening risks; and extreme caution should be exercised in such individuals insisting to fast.
Patients may be at higher or lower risk for fasting related complications depending on the number and extent of their risk factors.
Conditions associated with “very high,” “high,” “moderate,” and “low” risk for adverse events in patients with type 1 or type 2 diabetes who decide to fast during Ramadan are summarised in a table below.
Fasting for patients with diabetes represents an important personal decision that should be made in light of guidelines for religious exemptions and after careful consideration of the associated risks in consultation with health care providers. Most often, the medical recommendation will be not to undertake fasting.
However, patients who insist on fasting need to be guided on the associated risks of the fasting experience and techniques to decrease these risks.
Fasting during the month of Ramadan for Muslims imposes extra demands on the body that include abstinence from food and fluid intake during the period from dawn to sunset, as well as a reduction in meal frequency and alterations in the sleep-wakefulness cycle.
Management
The most important thing is to realise that care must be highly individualised and that the management plan will differ for each specific patient. There is no “coat that suits all”, and each person should have a management plan during the fasting period individually. This management plan needs to be revised with every fasting period, and even within the same fasting period. It should not be cast in stone.
Table showing characteristics of diabetes with risk during fasting.
Category of Risk | Disease States |
Very High Risk | · In the last three months, had severe low sugar · Gets low sugar without sensing that there is low sugar · Poor blood sugar control · Acute illness · Type 1 diabetes (insulin-dependent diabetes) · Performing intense physical labour · Pregnancy · Kidney failure on dialysis |
High Risk | · Moderate poor control (HbA1c more than > 9.5% · Kidney failure · Living alone and treated with insulin or sulfonylurea · Old age with ill health |
Moderate Risk | · Diabetes well controlled treated with tabs for diabetes that may cause low sugar |
Low Risk | · Well-controlled diabetes on medications that are not associated with low sugar |
Frequent monitoring of blood glucose
It is essential that patients have the means to monitor their blood glucose levels multiple times daily during the fasting period. This is critical in patients with type 1 diabetes and in patients with type 2 diabetes who require insulin. They should be educated about the checking of glucose in the blood and which levels are safe, and what intervention to use should the readings be outside the safe range (be high or low).
Continuous glucose monitoring (CGM) is now available in Uganda, although still costly. Patients may enquire about this from their healthcare providers.
Nutrition During Ramadan: There is a major change in the dietary pattern compared with other times of the year. Most health problems are likely to arise from an inappropriate diet or as a consequence of overeating and insufficient sleep.
Therefore, the diet during Ramadan for people with diabetes should not differ significantly from a healthy and balanced diet.
The nutritional advice should be tailored to their special needs and medical problems.
It should aim at maintaining a constant body weight. The common practice of ingesting large amounts of foods rich in carbohydrates and fats, especially at the sunset meal (Iftar), should be avoided. Ingesting large amounts of food at “breaking the fast” is a very common practice in Uganda.
Avoid excessive juices (with or without sugar added), excessive fruits and Katogo. Note that in terms of energy value, one finger of matooke is equivalent to two slices of family loaf of bread; and thus eating 4 – 6 ‘fingers’ of matooke is equivalent to eating 8 – 12 slices of family loaf of bread i.e. half a loaf alone!
This will overwhelm the mechanisms of the body to control the blood glucose. It is also important to remember that fruits are carbohydrates and can increase weight. Quantities of fruits should be measured and taken in the right quantities. The overall approach is to go heavier on the vegetables (approximately 5 servings) and lighter on the fruit (approximately 2 -3 servings) a day. Fruits should not be taken adlib; quantities and timings should be observed.
Because of the delay in digestion and absorption, ingestion of foods containing “complex” carbohydrates (slow-digesting foods – the vegetables) may be advisable at the predawn meal (Suhoor; Daku), which should be eaten as late as possible before the start of the daily fast. It is also recommended that fluid intake be increased during non-fasting hours.
Normal levels of physical activity may be maintained. However, excessive physical activity may lead to a higher risk of hypoglycemia (low sugar in the body) and should be avoided, particularly during the few hours before the sunset meal.
Quite commonly, multiple prayers are performed after the sunset meal; this generally involves repeated cycles of rising, kneeling, and bowing and should be considered a part of the daily exercise programme. In some patients with poorly controlled type 1 diabetes, exercise may paradoxically lead to severe hyperglycemia (high sugar in the blood).
Breaking the fast
All patients should understand that they must always and immediately end their fast if hypoglycemia (low glucose in the blood; less than 60 mg/dl [3.3 mmol/ l]) occurs because the blood glucose may drop further if there is a delay in treatment.
The fast should also be broken if blood glucose reaches less than 70 mg/dl (3.9 mmol/l) in the first few hours after the start of the fast, especially if insulin or tablets that lower sugar in the blood are taken at pre-dawn. Finally, the fast should be broken if blood glucose exceeds 300 mg/dl (16.7 mmol/l). Patients should avoid fasting on “sick days.”
Pre-Ramadan medical assessment
Many Muslims with diabetes are very passionate about fasting during Ramadan. This passion is a golden opportunity to empower people with diabetes for better management of their diabetes, not only during Ramadan but also throughout the year.
All patients with diabetes who wish to fast during Ramadan should prepare by undergoing a medical assessment and engaging in a structured education programme to undertake the fast as safely as possible. Ideally, this assessment should take place 1–2 months before Ramadan.
Specific attention should be devoted to patients’ overall well-being and to the control of their blood glucose, blood pressure, and lipids (fats in the blood, including Cholesterol and Triglycerides). Appropriate blood studies should be ordered and evaluated.
Specific medical advice must be provided to individual patients concerning the potential risks if they decide to fast.
During this assessment, necessary changes in diet or medication regimen should be made so that the patient initiates fasting while on a stable and effective program.
This assessment should also extend to those who do not wish to fast because they are often exposed to the risk of hypo (low sugar)- and hyperglycemia (high sugar) during Ramadan as a reflection of social habits encountered during the month.
Medications
The scope of this article does not allow discussion of medications. Suffice to mention that the details should be discussed with a health worker conversant with the management of diabetes and knowledgeable about the changes that follow fasting while taking medications. For fasting to be safe, it should be accompanied by an appropriate understanding of the patient regarding the medications and risks involved.
About the writers:
Silver Bahendeka is a Professor of Medicine and Endocrinology at the Uganda Martyrs University School of Medicine, and the Chair of the East Africa Diabetes Study Group (EADSG).
Silver.Bahendeka@eadsg.org
Sheikh Mohammad Ali Waiswa is the Deputy Mufti of Uganda.
sheikhwaiswamuhammad@gmail.com